How to make a beta cell divide
An ETH Zurich research team-in collaboration with Roche Pharmaceuticals- has discovered a hitherto unknown mechanism by which the insulin producing beta cells are negatively affected. This raises new hopes for pharmacologically stimulating these cells to divide and thus combating diabetes.
Bace1 is by no means an unknown enzyme. It is the protease cleaving the amyloid protein in the brain and is thereby significantly contributing to the pathogenesis of Alzheimer’s disease. About its close relative Bace2, however, we for a long time merely knew that it is not involved in this disease, as it is barely present in neurons. But now a research group led by Markus Stoffel, professor for Metabolic Diseases at The Institute of Molecular Systems Biology, ETH Zurich, has found both a “home” and a function for this orphan: The enzyme is primarily present in pancreatic beta cells and regulates the proliferation of this cell type.
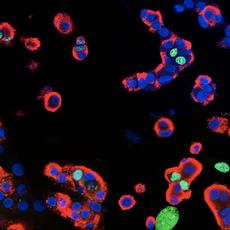
Bace2, just like Bace1, is a cellular pair of scissors, a so-called membrane protease. The enzyme is embedded into the membrane, cleaves cell surface proteins and thereby inactivates them. The investigators determined one of the possibly most important substrates of Bace2: the beta cell growth-promoting protein “Tmem27”. When Tmem27 is removed by Bace2 activity, the cells are only dividing slowly or not at all. Or conversely: the less active Bace2 is, the faster the cells are proliferating.
Beta cells are essential for the regulation of blood sugar levels in the body. They produce insulin, which triggers glucose uptake in many tissues. Once a critical amount of beta cells is damaged or lost, we develop full blown diabetes.
Beta cells prosper without the protease
To test the hypothesis that the inactivation of this membrane protease would be beneficial, the team analyzed genetically modified mice that lack active Bace2. Indeed, the researchers observed augmented Tmem27 levels in the membranes of the beta cells. Additionally, the mice exhibited increased beta cell mass and insulin secretion.
The investigators also found a way to block active Bace2: within the compound library of the pharmaceutical company Roche they identified a specific inhibitor for this protease. When diabetic mice were treated with this substance, their beta cells divided at a faster rate. Their glucose handling improved, indicating that the newly produced cells were indeed secreting more insulin. Diabetics have good grounds for optimism as well: Bace2 and Tmem27 are present in human beta cells, so that these patients too may at some point benefit from Bace2 inhibition
RNA interference sheds light on Bace2
This mechanism was unraveled in a quite straightforward manner: The researchers knew that an unknown protease had to cut Tmem27. So they embarked on the search for this enzyme, in the hope to find a way to increase Tmem27 levels and thereby beta cell mass and function. The investigators systematically investigated the proteases present in the beta cell. Using a technique called RNA interference they inactivated the specific genes, amongst them the gene for Bace2. This is when they realized that preventing Bace2 expression led to the absence of Tmem27 cleavage products and an enrichment of the intact version of the protein. “We had absolutely no reason to expect that Bace2 would be the protease“, says Markus Stoffel retrospectively.
Tmem27 may very well not be the only target of Bace2. The researchers are convinced that a combination of different substrates contribute to cell proliferation and insulin secretion. Also, in their most recent paper that was published in „Cell Metabolism“ the scientists state that Bace2 inhibition leads to imminent Tmem27 stabilization and to accelerated cell division within a few days. However, the increase in insulin secretion was only observed after a much longer time period. This may mean that upon increasing in mass, the beta cells have to be reprogrammed and rearranged within the pancreatic islet such that the increased insulin secretion can ensue. Physiologically it makes sense for the body to have these additional layers of control: hypoglycemia would be the consequence if all of a sudden too much insulin were secreted, and that may be just as fatal as diabetes
Bace2, important for keeping the balance?
But why do we possess Bace2 at all? “This enzyme is not the bad guy as such - we all live with it”, says Daria Esterházy, the main author of the study. Beta cell mass fluctuates and adjusts to new situations in the course of life. For example, it increases during pregnancy but shrinks again afterwards. Bace2 could be involved in such processes. However, Bace2 activity is likely to be a real disadvantage for people who do already have decreased beta cell mass.
It is a
long way until these findings may be translated into an anti-diabetic therapy.
Esterházy hopes that the situation for type 1 diabetics can also be improved.
Typically a few beta cells are left in these patients. “If these cells could be
stimulated to divide, that would be fantastic“, says the ETH scientist.
Literature:
Esterhazy D et al. Bace2 is a Beta cell-enriched Protease that regulates pancreatic beta cell function and mass. Cell Metabolism (2011), doi: 10.1016/j.cmet.2011.06.018
- 10.09.11: Betazellen zur Teilung angeregt: Gute Sache
- 09.09.11: Betazellen zur Teilung angeregt: Hurra!







READER COMMENTS